TIM-3 therapy for Alzheimer’s represents a groundbreaking approach in the quest for effective Alzheimer’s disease treatment. Recent studies have shown that targeting the TIM-3 checkpoint molecule can enhance the function of microglia, the brain’s immune cells, allowing them to clear harmful amyloid plaques associated with Alzheimer’s. By inhibiting TIM-3, researchers observed remarkable cognitive improvement in mice previously afflicted by memory loss due to plaque accumulation. This innovative therapy not only reshapes the immune response in the brain but also holds the potential to revolutionize how we combat the effects of Alzheimer’s disease. As scientists continue to explore the intricate relationship between TIM-3 and Alzheimer’s, there is renewed hope for developing effective solutions to combat this devastating condition.
The investigation into TIM-3 treatment for Alzheimer’s disease highlights an exciting intersection of neuroscience and immunology. This approach is grounded in the understanding that microglial cells, which act as the brain’s immune defenders, can be revitalized to attack the amyloid plaques that dominate Alzheimer’s pathology. By deactivating the TIM-3 inhibitor, researchers have seen promising signs of recovery and cognitive enhancement in model organisms. This line of research is paving the way for breakthroughs in addressing the underlying mechanisms driving Alzheimer’s progression, offering new avenues for therapeutic intervention. As such, the implications of TIM-3 modulation extend not only to Alzheimer’s but also potentially illuminate broader strategies for addressing various neurodegenerative conditions.
Understanding TIM-3 and Its Role in Alzheimer’s Disease
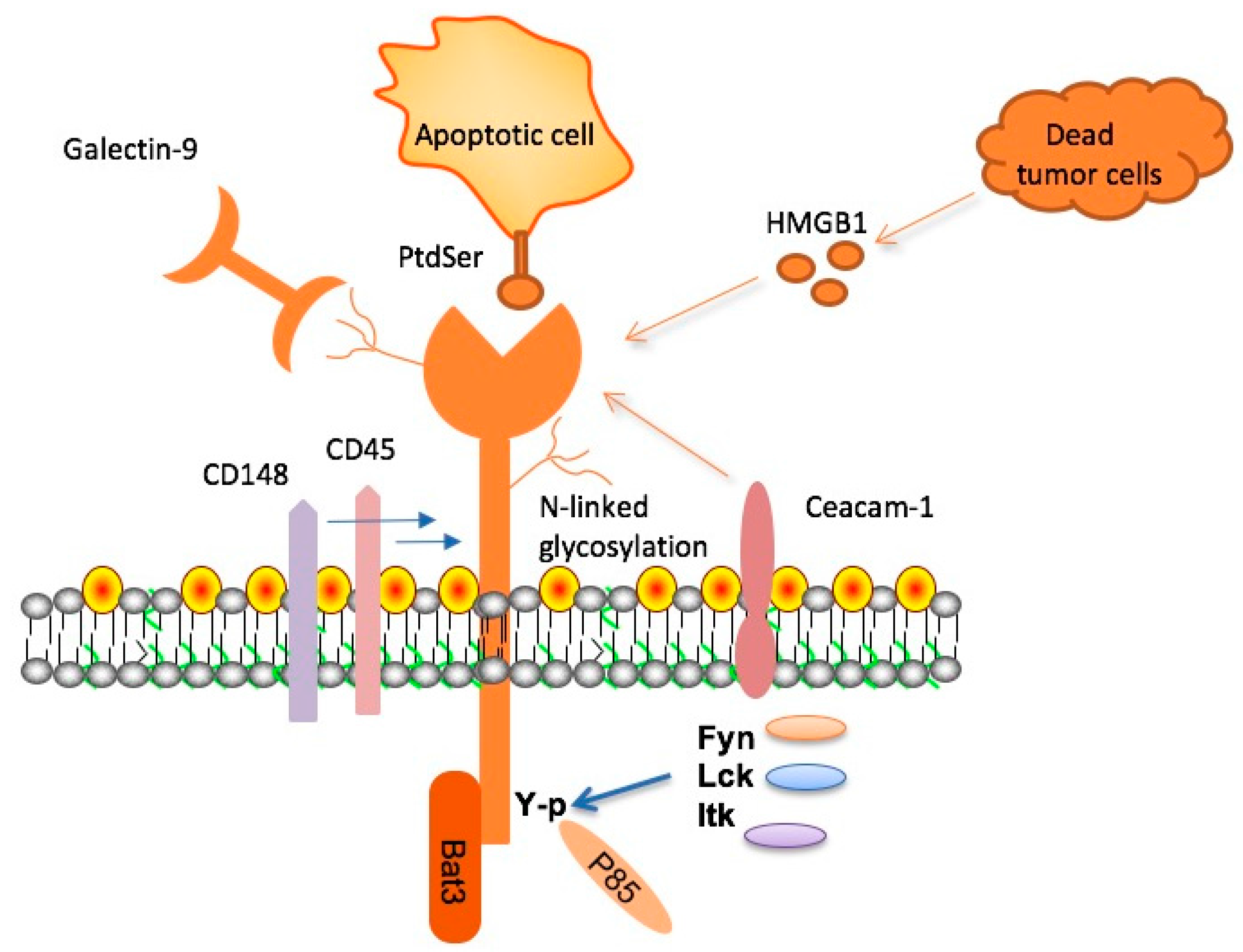
TIM-3, or T-cell immunoglobulin and mucin-domain containing-3, has emerged as a critical molecule in the study of Alzheimer’s disease (AD). As the genetic underpinnings of late-onset Alzheimer’s have been explored, TIM-3 has been identified as a significant risk factor, with polymorphisms in the HAVCR2 gene linked to increased disease vulnerability. Research indicates that TIM-3 acts as an inhibitory checkpoint molecule that limits the activity of microglia— the brain’s primary immune cells — rendering them less effective at clearing harmful amyloid plaques that accumulate in Alzheimer’s patients.
In essence, mutated or overexpressed TIM-3 on microglia results in a homeostatic state, where these crucial cells become less aggressive in their response to the plaque buildup. Instead of actively engaging and removing amyloid beta, the microglia remain dormant and incapable of sustaining optimal immune functionality in the brain. This lack of responsiveness not only exacerbates the buildup of toxic plaques but also correlates with cognitive decline, illustrating the dual role TIM-3 plays as both a regulatory molecule and a potential therapeutic target.
Microglia and Their Functions in Alzheimer’s Disease
Microglia are integral to maintaining brain health, functioning as the first line of defense against pathogens and debris that threaten neural integrity. In the context of Alzheimer’s disease, these immune cells undergo critical shifts as age progresses and disease pathologies intensify. While microglia have the capability to prune unnecessary synaptic connections during cognitive development, their impaired function in Alzheimer’s disease leads to accumulation of plaques, hindering cognitive development and memory consolidation.
Moreover, when TIM-3 expression peaks in older individuals, it essentially restrains microglial activity, compelling them into a homeostatic state where they are no longer able to phagocytize and clear amyloid plaques or cellular debris effectively. This situation highlights a pivotal challenge in Alzheimer’s treatment: how to invigorate these immune cells to fulfill their roles without compromising their regulatory functions to prevent autoimmunity.
The Intersection of Cancer Immunotherapy and Alzheimer’s Treatment
Recent breakthroughs in cancer immunotherapy have provided a novel lens through which Alzheimer’s treatments can be envisioned. An anti-TIM-3 antibody, which has been utilized successfully in eradicating some types of tumors, shows promise for reversing cognitive decline in Alzheimer’s patients by reactivating microglial functions previously incapacitated by the molecule’s inhibitory effects. This convergence of strategies suggests that lessons learned from oncology might be effectively applied to neurodegenerative diseases, potentially paving the way for innovative therapies targeted at Alzheimer’s.
By inhibiting the activity of TIM-3, the intention is to free microglia from the confines of their checkpoint roles, allowing them to resume their critical functions in clearing amyloid plaques. Employing targeted agents to disrupt TIM-3 could restore the immune response that has faltered due to aging and Alzheimer’s pathology, ultimately enhancing cognitive functions and rejuvenating memory capabilities in affected individuals.
Clinical Implications of TIM-3 Therapy for Alzheimer’s
The therapeutic approach of utilizing TIM-3 inhibition offers a pathway to rejuvenate cognitive functions in Alzheimer’s disease. Preliminary findings from experiments with genetically engineered mice demonstrate that deleting the TIM-3 gene can significantly improve plaque clearance by enhancing microglia efficiency. These insights indicate a desperate need to progress this research from preclinical models into human clinical trials, where the potential of TIM-3-targeting therapies could be translated into meaningful cognitive improvements for patients suffering from Alzheimer’s.
However, transitioning from laboratory results to real-world applications necessitates meticulous trials to assess the safety and efficacy of anti-TIM-3 treatment strategies in humans. Critical evaluations will focus on determining the optimal dosages, understanding the side effects, and monitoring responsiveness in older populations who exhibit varying degrees of cognitive impairment. The promise of TIM-3 therapy for Alzheimer’s could revolutionize current treatment paradigms, signaling a new era where previously untreatable cognitive decline might now be addressed head-on.
The Future of Alzheimer’s Disease Research and TIM-3
As the understanding of Alzheimer’s disease progresses, the role of TIM-3 has emerged as a transformative concept in the field. The potential for exploiting this checkpoint molecule signifies a broadened horizon for innovative treatments that challenge traditional paradigms. Moving forward, ongoing research will aim to elucidate the specific mechanisms through which TIM-3 modulates microglial responses to plaque accumulation and how these insights can be translated into viable therapy options.
Furthermore, collaborative endeavors involving multidisciplinary teams are essential to unravel the complexity surrounding TIM-3 function and its implications in Alzheimer’s. Initiatives that integrate molecular biology with clinical studies will shed light on therapeutic efficacy and open doors to novel interventions. The goal is to provide tangible solutions for combating Alzheimer’s disease, thereby improving the quality of life for millions affected by this devastating condition.
Investigating Cognitive Improvement in Alzheimer’s Models
When evaluating cognitive decline in preclinical settings, the promise of TIM-3 manipulation hinges on defined models that replicate the pathological features of Alzheimer’s disease in humans. In trials involving laboratory mice, researchers have documented notable enhancements in behavior and memory following TIM-3 inhibition. These findings have highlighted the significant link between immune regulation, plaque control, and cognitive performance, drawing attention to the transformative potential of an immune-oriented strategy in Alzheimer’s treatment.
Moreover, it has been shown that mice lacking TIM-3 showed improvements not just quantitatively in terms of plaque reduction, but qualitatively, altering the nature of the plaques themselves. This dual benefit — clearing both the quantity and toxicity of plaques — has profound implications for the treatment of Alzheimer’s, suggesting that cognitive improvement could extend beyond mere plaque clearance to encompass broader neuroprotective effects when TIM-3 is effectively targeted.
The Role of Checkpoint Molecules in Immune Response in Alzheimer’s
Checkpoint molecules, which include TIM-3, play pivotal roles in modulating the immune response, preventing overactivation that could harm the host. In the context of Alzheimer’s, the regulation provided by TIM-3 becomes detrimental when it guards microglia against necessary actions to combat amyloid plaques. Understanding the balance of immune regulation through checkpoint molecules is critical as researchers seek to manipulate these pathways to restore balance in the Alzheimer’s-affected brain.
In essence, checkpoint inhibitors, such as anti-TIM-3 therapies, could unlock potential avenues previously closed to Alzheimer’s treatment. By navigating the delicate interplay between immune activation and regulation, these therapies may reposition the immune response in a way that shifts the trajectory of cognitive decline, allowing for more effective interventions in the fight against Alzheimer’s disease.
Conclusion: Potential of TIM-3 Therapy for Alzheimer’s Disease
The future of Alzheimer’s disease therapy is increasingly unified through the lens of immune modulation, with TIM-3 standing at the forefront. There remains a growing recognition of the importance of microglial function, and targeting TIM-3 as a therapeutic strategy presents a compelling opportunity for breaking the mold of current treatment approaches. As researchers refine their understanding of TIM-3’s biological roles, there is a real possibility that this could translate into significant cognitive benefits for individuals battling Alzheimer’s.
In closing, the integrated strategy of utilizing existing knowledge from cancer therapies may be a crucial component in developing next-generation treatments for Alzheimer’s disease. As studies progress towards human applications, the ongoing insights into TIM-3’s role will undoubtedly illuminate critical pathways for drug development, promising a brighter outlook for Alzheimer’s patients and their families.
Frequently Asked Questions
What is TIM-3 therapy for Alzheimer’s disease and how does it work?
TIM-3 therapy for Alzheimer’s disease involves targeting the TIM-3 molecule to enhance the immune response of brain microglia. By inhibiting TIM-3, microglia can effectively clear amyloid plaques that are linked to Alzheimer’s, leading to cognitive improvements, as demonstrated in animal studies.
How effective is TIM-3 therapy for cognitive improvement in Alzheimer’s patients?
Current research indicates that TIM-3 therapy has shown promise in animal models, leading to significant cognitive improvements in mice with Alzheimer’s disease. While human trials are still needed, the potential benefits suggest that TIM-3 therapy could be a new avenue for Alzheimer’s disease treatment.
What role do microglia play in TIM-3 therapy for Alzheimer’s disease?
Microglia are the brain’s immune cells responsible for clearing amyloid plaques. TIM-3 therapy aims to activate microglia by inhibiting the TIM-3 protein, allowing them to attack and remove these plaques, which is crucial for slowing the progression of Alzheimer’s disease.
Can TIM-3 therapy be used in conjunction with other Alzheimer’s disease treatments?
It is possible that TIM-3 therapy for Alzheimer’s could complement existing treatments. Since it uniquely targets the immune system’s ability to clear plaques, combining it with other therapies may enhance overall effectiveness and address different aspects of Alzheimer’s pathology.
What is the potential of repurposing TIM-3 antibodies for Alzheimer’s disease treatment?
Repurposing TIM-3 antibodies for Alzheimer’s disease treatment shows significant potential due to their selective expression in microglia. This offers a targeted approach that could reduce plaque accumulation without the vascular risks associated with traditional anti-amyloid therapies.
Are there any risks associated with TIM-3 therapy for Alzheimer’s disease?
While TIM-3 therapy for Alzheimer’s disease holds promise, potential risks could involve unintended immune responses or effects on other brain functions. Ongoing research is essential to evaluate the safety and efficacy of this treatment before human application.
What is the connection between TIM-3 and Alzheimer’s disease genetic risk factors?
Genetic studies have identified polymorphisms in the TIM-3 gene as significant risk factors for late-onset Alzheimer’s disease, suggesting that variations in TIM-3 expression may influence the susceptibility to developing Alzheimer’s and the progression of the disease.
How does TIM-3 therapy compare to traditional Alzheimer’s treatments?
TIM-3 therapy differs from traditional Alzheimer’s treatments by directly enhancing the brain’s immune response to clear plaques, rather than solely targeting the amyloid beta protein. This innovative approach may provide a new mechanism of action compared to existing therapies.
| Key Point | Details |
|---|---|
| Study Focus | Investigates the role of TIM-3 in late-onset Alzheimer’s disease and its potential for therapy. |
| Main Finding | Deleting TIM-3 enhances the ability of microglia to clear amyloid plaques, which improves memory in mice. |
| Significance of TIM-3 | TIM-3 is a checkpoint molecule that inhibits the immune response, preventing microglia from attacking plaques. |
| Cognitive Assessment | Mice with Alzheimer’s show impaired memory; plaque clearance leads to improved memory and fear responses. |
| Future Implications | Potential development of TIM-3 therapy could lead to new Alzheimer’s treatments using antibodies or small molecules. |
| Next Steps | Testing human anti-TIM-3 antibodies in mouse models to assess plaque prevention. |
Summary
TIM-3 therapy for Alzheimer’s is showing promising potential as a new approach in treating this devastating disease. By targeting the TIM-3 protein, researchers aim to enhance microglia activity, enabling them to clear amyloid plaques that contribute to cognitive decline. The findings from recent studies indicate that manipulating TIM-3 expression can lead to improvements in memory functions in mice, which serves as a hopeful avenue for developing effective therapeutics for Alzheimer’s disease.